Customized medications possible boon for pediatric, geriatric patients
More than 40% of older Americans take five or more prescription drugs a day, and nearly 20% take 10 or more. What if there was a way to combine those medications into one easy-to-track pill?
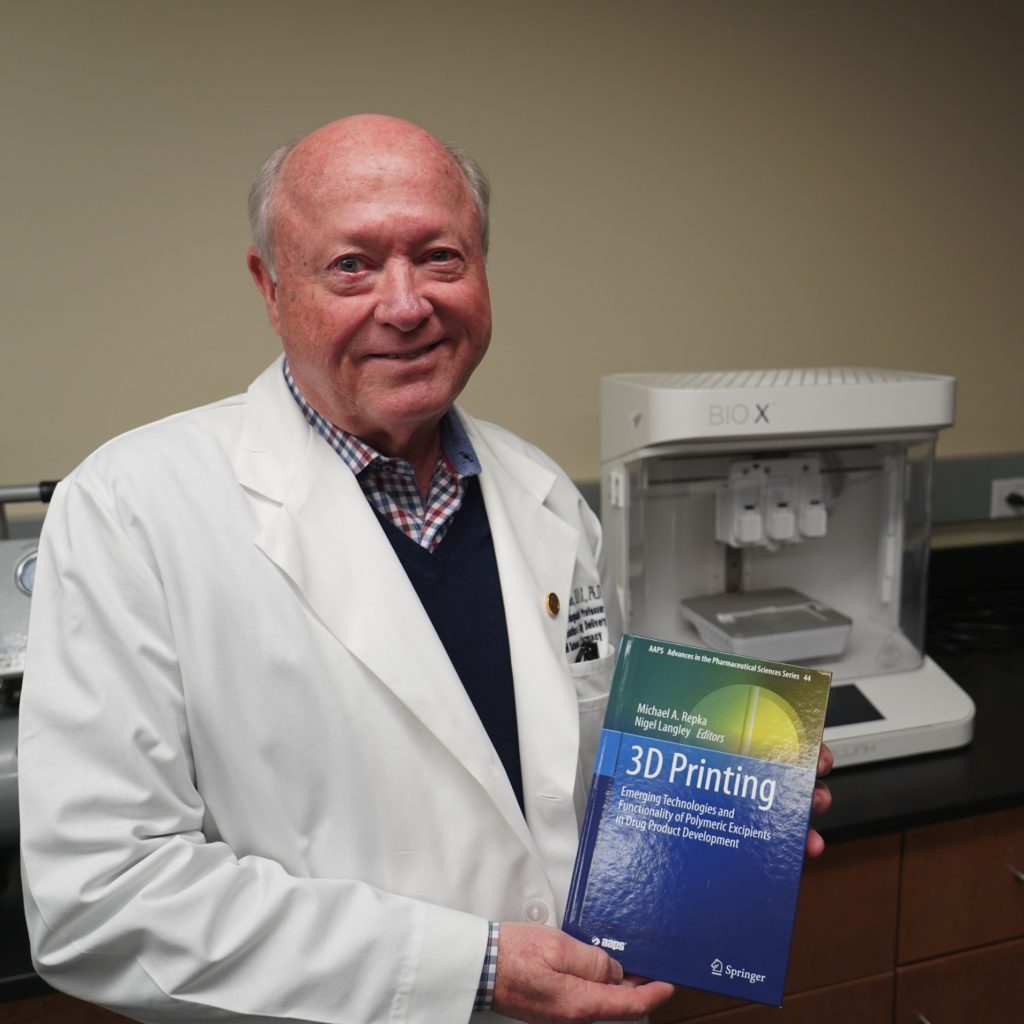
The use of 3D printing to create customized pills could do just that, say University of Mississippi pharmacy professor Michael Repka and two alumni of the School of Pharmacy. Repka worked with Sagar Narala and Dinesh Nyavanandi, who recently completed doctoral degrees in pharmaceutical science, to outline the plan in a chapter from “3D Printing: Emerging Technologies and Functionality of Polymeric Excipients in Drug Product Development” (Springer Cham, 2024).
Using 3D printing, medications can be tailored by size, shape, dosage and content, customizing each tablet to the patient, said Repka, distinguished professor of pharmaceutics and drug delivery.
“Pharmaceutical companies have a one-size-fits-all approach to dosage, but that doesn’t work for everybody,” he said. “With this, we can tailor that dosage to what the patient needs.”
Being able to customize the size of medications could also benefit geriatric and pediatric patients, Nyavanandi said. In one study, 69% of geriatric patients admitted to skipping dosages because the pills were too difficult to swallow.
“There are many limitations with conventional medications, like the size of the tablet or capsule,” he said. “For pediatric and geriatric patients, the size of the tablet is a big challenge for them.
“Many of the pediatric and geriatric population will skip their medication because of the size of the tablet.”
With 3D printing, however, pharmacists can print not only smaller doses, but also customize the color or print the medication in the shape of a gummy bear or another familiar shape to help encourage young children, Repka said.
The process could also eliminate some issues of medications expiring on the shelf, Narala said.
“For every medication, stability and storage are the most common challenges,” Narala said. “If we use 3D-printing medication, it is made when it is needed in a pharmacy setting, and we can avoid the associated stability or storage issues. 3D printing can avoid large-scale manufacturing, particularly beneficial for drugs with limited markets.”
Although the idea of 3D printing medication is not new – the U.S. Food and Drug Administration approved the United States’ first printed medication in 2015 – the process remains too slow and costly for widespread use, Repka said.
In the chapter, Nyavanandi, Repka and Narala explore a method of creating drug-loaded polymer filaments that can be used as the “ink” in a 3D printer, Repka said.
The authors call for more investment and study into this technology, which Nyavanandi said could revolutionize the pharmaceutical industry.
“Every once in a while, there is a new technology that will be introduced to the market, but not every new technology is free of limitations,” Nyavanandi said. “There are currently limitations (to 3D printing), but if this 3D printing research goes well and gets implemented into the pharmacies, it will create a revolution in the pharmaceutical industry.”
If researchers can speed up the process of printing medication, printers could be installed in pharmacies, allowing local pharmacists to print medication on an as-needed basis, Repka said. This could streamline the process of getting medication to the patients who need it, he said.
“To me, it’s mind-blowing that this is going to be happening,” Repka said. “People have to know what they’re doing to print it, but the pharmacists working in the field right now can do this, and it actually makes it easier for them.”
By Clara Turnage