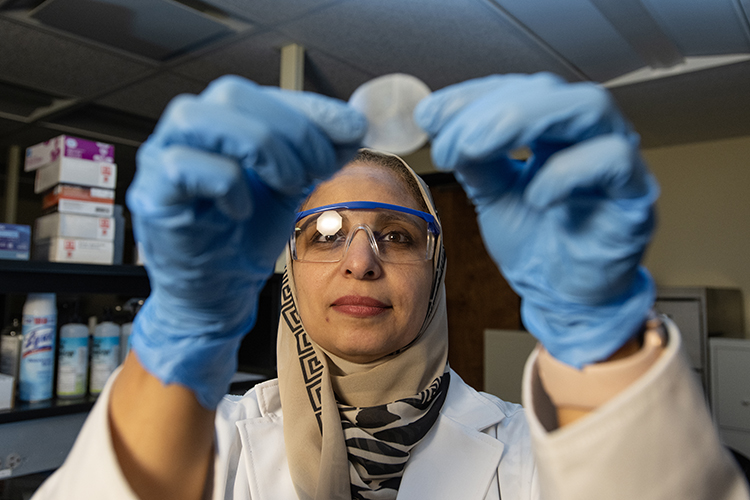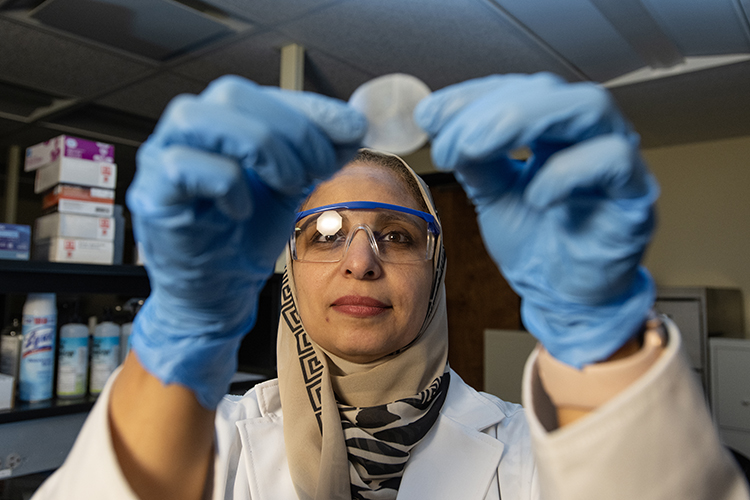
Eman Ashour, assistant professor of pharmaceutics and drug delivery, examines a 3D-printed film developed by University of Mississippi researchers that could improve drug delivery options for cervical cancer patients. Photo by Thomas Graning/Ole Miss Digital Imaging Services
Vaginal delivery method addresses challenges with oral medication
Scientists at the University of Mississippi are developing a vaginal, 3D-printed film that could improve drug delivery options for cervical cancer patients.
Each year in the U.S., about 11,500 cases of cervical cancer are diagnosed and some 4,000 women die of the disease, according to the Centers for Disease Control and Prevention. Mississippi has the nation’s second-highest age-adjusted cervical cancer mortality rate at 3.4 deaths per 100,000 women and girls annually.
While most medications are oral, this route has side effects, absorption issues and is not well received by patients.
UM researchers explored the complexities and benefits of administering the drug disulfiram vaginally. The International Journal of Pharmaceutics published their findings in March. Approved by the U.S. Food and Drug Administration to treat alcoholism, disulfiram has shown promise for treating cancer.
“Vaginal drug delivery offers targeted, localized delivery,” said Eman Ashour, assistant professor of pharmaceutics and drug delivery. “The vaginal film’s sticking properties help extend the film’s retention and the drug release, which is an added advantage.”
Ahmed Almotairy developed the idea for his doctoral dissertation while at Ole Miss. Almotairy is an assistant professor of pharmaceutics and pharmaceutical technology at Taibah University in Saudi Arabia.
“I was enlightened by the published work on this particular drug,” said Almotairy, who was lead investigator. “In terms of patient treatments, disulfiram showed promising results against many types of cancer.”
Researchers combined hot-melt extrusion and 3D printing to design patient-specific doses. Hot-melt extrusion, or HME, involves melting a material and reshaping it as it cools. The scientists used HME to produce drug-loaded filaments, or threads of material, which were then used to 3D print the desired dose.
“Our work at the end is meant to improve the patient’s quality of life,” Almotairy said.
Disulfiram is heat-sensitive, which initially posed a problem for vaginal delivery. The research team overcame this issue by optimizing the drug’s design and the HME’s processing temperatures.
The film makes it possible to deliver medications directly to the target site because the cervix is easily accessible through the vagina, Ashour said. This technology has a wide range of implications; anti-fungal, antimicrobial, anti-cancer and hormone drugs are also promising drug candidates for vaginal delivery.
“The results of this user-inspired study will contribute to improving patient outcomes and treatment alternatives,” she said. “We hope to build new technologies based on this project’s success and explore other disease states and uses in the future.”
This project was partially supported by the National Institute of General Medical Sciences (Grant Number P30GM122733), which is a component of the National Institutes of Health serving as one of its Centers of Biomedical Research Excellence.
By Erin Garrett